Journal of Clinical Cardiology and Cardiovascular Diagnosis
Review Article
The Cardiometabolic Continuum, A Practical and Early Preventive Strategy for Cardiometabolic Diseases
1Clinical cardiologist, medical writer, Venezuelan Society of Cardiology, Claret Outpatient Clinic, Caracas, Venezuela
Abstract
Introduction
Cardiometabolic continuum, background
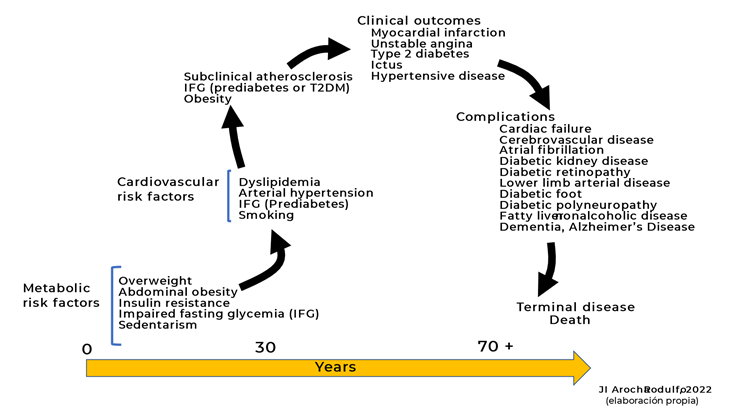
Figure 1 :Life cycle of the cardiometabolic continuum
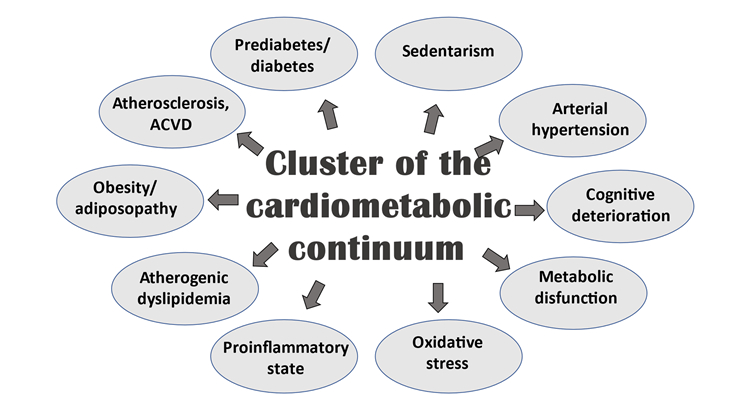
Figure 2: Complexity of the cardiometabolic continuum
The epidemic of overweight/obesity and sedentary lifestyle in most countries has drawn attention to certain pathophysiological mechanisms, barely previously considered in the development and progression of atherosclerosis, as the main pathophysiological underpinning of CVD (4,6,7,8).
Under regular physiological conditions, insulin regulates glucose homeostasis by enhancing glucose disposal in insulin-sensitive tissues, while also regulating delivery of nutrients through its vasodilation actions on small feed arteries (10-12). Specifically, insulin-mediated production of nitric oxide (NO) from the vascular endothelium leads to increased blood flow enhancing disposal of glucose. Typically, insulin resistance is considered as a decrease in sensitivity or responsiveness to the metabolic actions of insulin, including insulin-mediated glucose disposal (11,12). However, a decreased sensitivity to the normal vascular actions of insulin, especially diminished nitric oxide production, plays an additional important role in the development of CVD in states of insulin resistance through increases in vascular stiffness (10-13).
Both overweight/obesity and sedentary lifestyle have hyperinsulinemia as a common denominator, with its consequent resistance to insulin. Such resistance begets alterations in the metabolism of carbohydrates and lipids, giving rise to a more complicated situation where the correction or modification of the initial alteration change the consequences derived from them insubstantially or not at all (14,15). Numerous and complex pathogenic pathways link obesity with the development of insulin resistance, including chronic inflammation, mitochondrial dysfunction (with the associated production of reactive oxygen species and endoplasmic reticulum stress), gut microbiota dysbiosis and adipose extracellular matrix remodelling (16-18). Insulin resistance itself plays a key role in the development of metabolic dysfunction, including hypertension, dyslipidaemia and dysglycaemia. It, furthermore, promotes weight gain related to secondary hyperinsulinaemia, with a resulting vicious cycle of worsening insulin resistance and its metabolic sequelae (16,18).
This observation makes it possible to highlight the relevance of a very important, but generally unnoticed or poorly attended, factor: time; and the reason is simple: since these modifications in metabolism are silent for many years until they become chronic and established with organic damage or clinical manifestation, untimely clinical intervention does not allow for sufficient and radical changes to be made to correct the organic consequences of such imbalances (19). This means that, with rare exceptions, management for cardiometabolic risk factors (CMRF) and ACVD is a lifelong endeavor, since drugs and changes in lifestyle only slow down the rate of progression of the cardiovascular disease, and perhaps may only reduce the risk of a cardio or cerebrovascular event (20).
It is currently accepted that each of the events in this continuum are the result of common processes participating in multiple steps through it, that may or may not be accompanied by cognitive impairment and, as the disease progresses, results in dementia and cardiac embolism or cause end-stage kidney damage and failure. In terms of prevention, the CMC is very practical, versatile, and essential in understanding a series of concatenated events that cover the transition from the appearance of CMRF, including metabolic ones, to the development of a clinical, cardiovascular, metabolic condition, or both, with the possible inclusion of another additional pathology in the course of the evolution to the outcome.
For many decades obesity has been considered as the result of a lack of discipline and higher caloric intake, in addition to the lack of necessary physical activity. This has led to certain negative attitudes to such as stigmatization of subjects with obesity and social restriction (21). Although obesity is a positive energy balance, it, in fact, comprises a complex and coordinated integration of indicators to the appetite with a chronic signaling of the energy state (22). Unfortunately, many healthcare professionals, as well as some patients, consider obesity to be a lifestyle disease, suffered by people lacking the willpower to self-regulate their food intake. But obesity is really a very complex disease with many causes, chronic and progressive, thus it should also be treated like other complex, chronic, progressive diseases; moreover, the degree of obesity is associated with complex multimorbidity, especially T2DM, in a dose–response relationship (23,24). These findings highlight the devastating impact of obesity’s association with an increasing burden of complex multimorbidity, including cardiometabolic, blood pressure, digestive, respiratory, neurological, musculoskeletal, and infectious diseases (23). This implies, mainly, that treatments must be continued on a long-term basis to avoid, delay, or minimize the complications.
The different components of energy intake and its balance regulation are factors regulated by homeostatic and non-homeostatic neural mechanisms (22,25).
Circulating hormones and vagal stimuli inform the central nervous system (CNS) about the nutritional and energy status of the entire organism. Leptin and insulin are known to be involved in the long-term regulation of energy balance, while gastrointestinal (GI) hormones and vagal afferent branches represent short-term regulatory mechanisms (26). Obesity, impaired fasting blood glucose (IFBG or prediabetes) and T2DM originally made up the group of cardiometabolic diseases; due to the accelerated growth of their prevalence, the close relationship between them with ACVD has been better understood (27). Subclinical atherosclerosis, physical inactivity, or sedentary lifestyle with all its cluster of metabolic alterations, sarcopenia, and nonalcoholic fatty liver (NAFLD) have been added to the cardiometabolic conditions. In most of these situations, the pathophysiological substrate is insulin resistance; it is not uncommon, however, for several of them to coexist, with or without arterial hypertension, which is the fatal combination to promote the progression of atherosclerosis and CVD (5,28,29). Furthermore, it must be considered that all these conditions mentioned favor the development of cognitive deterioration and dementia (30,31), an end point currently appearing at earlier ages and in a greater number of people.
Of course, any intervention, positive or negative, in CMC can modify the progression and outcomes of CVD in one way or another, as shown in Figure 1.
Cardiometabolic prevention since early age
As consequence of the description above mentioned, the prevention of cardiovascular disease must be initiated with impending metabolic risk factors such as overweight/obesity, impaired fasting glucose, or impaired glucose tolerance, sedentary behavior; these factors are usually present from the first decade of an individual’s life (19).
Extending routine systematic assessment from cardiovascular risk to cardiometabolic risk – that is, risk for developing ACVD and/or T2DM – and increasing the understanding of the basic mechanisms that regulate energy balance and metabolic risk factors, are needed to address the spread of epidemic of ACVD. Molecular and environmental conditions leading to cardiometabolic risk in early life, provide a challenge to develop effective prevention and intervention strategies to reduce the risk and modify the cardiometabolic continuum from a very early age, in order to yield earlier and greater benefits in reducing future cardiometabolic morbidity and mortality (19,32).
The main takeaway is the need for the healthcare profession to develop a
more empathetic and helpful approach to overweight/obesity and sedentarism, so patients feel encouraged to make changes in their lifestyle and gain better understanding how to go through them. It is important to note that if better lifestyle advice helps young people to avoid future cardiometabolic risk (by slowing or ceasing weight gain, losing weight, and increasing the time invested in moderate to vigorous physical activities), the potential long-term benefits to be reaped by delaying or preventing a range of clinical outcomes would be considerable (4,7,8,32).
The alarming growing in metabolic conditions presents substantial challenges to healthcare policies; it should serve as a call to improve prevention of cardiovascular disease by better targeting those at risk. At the same time, improving advice on lifestyle changes in clinical care towards sustainable better cardiometabolic health through life spam is a must (7,8,32).
Such lifestyle changes can lessen risks for several cardiometabolic diseases, including cardiovascular diseases, T2DM and non-alcoholic fatty liver disease, plus potentially some cancers, as well as improve quality of life. Public health strategies have major benefits in reducing populations’ risks for cardiometabolic diseases by, for example, taxing sugar-rich beverages, more areas to sport and massive education through social media (33).
Cardiometabolic prevention strategies offer a wider chronological window, as it can be applied from an early age and, thus, modify unhealthy lifestyle habits efficiently and permanently, without requiring the investment of huge amounts of money. Furthermore, this would widen the range of healthcare specialists that can be brought onboard in the application of said strategies, including paediatricians, adolescent health specialists, primary care physicians or general physicians.
Briefly, cardiometabolic prevention precedes and complement the cardiovascular prevention across a wide spectrum of action.
Results
Materials and Reagents
Calcium fluoride (Sigma), used as an ionophore, Ag(I)S and CuS were commercially obtained. Anion and cation solutions (Merck) were obtained from solid salts. All solutions were prepared using twice purified water.
Instruments
An external Ag/AgCl reference electrode with a Jenway 3040 pH/ion meter was used for potential measurement. Potential values were measured at room temperature.
Preparation of fluoride selective electrode
A certain amount of the salt or salt mixture of Ag(I)S, CuS and CaF2 (10–15 mg) was taken and pellets were made by holding first under a pressure of 1940 atm for 1min, then pressure was increased to 7760 atm by adding each time 1940 atm for 1min. The pellets of 7mmdiameter were sealed with epoxy resin (0.7 g epoxy and 0.9 ghardener). To obtain a good sealing the epoxy resin on the edge of the tubing had to wait for about 10 min and then the pellet was sealed. One day after the pellet was sealed a silver wire is connected. For this purpose, the inside of the glass tube was filled to about 1 cm with a mixture of 0.5 g graphite powder and epoxy resin. The electrode prepared had to wait for about 2 days so that the resin can get dry. The surface of the electrode is washed and then polished with a soft paper [10].
Preparation of teeth samples
Four dental samples were taken from the faculty of dentistry. Tooth samples were kept in 5ml TISAB II (Total Ionic Strength Adjustments Buffer) for 24 hours. The amount of fluoride passing into the solution was measured using an electrode.
Discussion
Due to the abundant documentation on the cardiometabolic issue derived from the numerous observational, epidemiological, intervention and clinical studies, the most effective strategy seems to be the early detection and treatment of the risk factors that trigger CMC as the only way to slow, stop or delay the onset and/or progression of CVD (19,34). Consequently, emphasis must be centered on primordial prevention (avoiding the appearance of risk factors) or on primary prevention (avoiding the damage caused by the risk factors present). In this regard, primary care physicians, general practitioners and doctors who are not specialists in the cardiometabolic approach are key since they receive most of the patients for the first time with some disorders of this type. Hence the importance of conceptualization as a continuum, as it is easily assimilated by the doctor and understandable to the patient as it is a vision of the problem marked by its progression over time.
The unbridled growth in the prevalence of overweight and obesity, especially in childhood and adolescence, will surely force the modification of the undergraduate and postgraduate studies in medicine, for an academic preparation in the cardiometabolic area and especially in nutrition, where it has been possible to objectify a deficiency in this knowledge in different published evaluations (35,36).
The fact that childhood obesity has gone from being a rare event to a common occurrence, with its repercussions traceable to adulthood is very alarming; so, the characterization of obesity as a matter of numbers must stop; it is essential that it be approached as a complex disease whose negative effects do not completely disappear with weight loss. In fact, obese children are five times more likely to remain obese than adults, with all attendant problems (37); moreover, many of these obese children and adolescents carry on elevated glycemic values or prediabetes resulting in earlier exposure to cardiometabolic consequences and, ultimately, long-term complications (38,39). In fact, as the prevalence rate of childhood obesity increases, a similar increase in the future burden of ACVD and T2DM is expected; therefore, policies aimed at reforming/eliminating the obesogenic environment in children and adolescents are crucial for health in future years and are an excellent long-term investment (40).
A recent cross-sectional study (41) showed that the association between body mass index (BMI) and diabetes risk in low-income and middle-income countries (LMICs) is subject to substantial regional variability; a higher risk of diabetes was observed at a BMI of 23 kg/m2 or higher, with a 43% greater risk of diabetes for men and a 41% greater risk for women compared with a BMI of 18.5-22.9 kg/m2. The risk of diabetes is greater at lower BMI thresholds and at younger ages than reflected in currently used BMI cutoffs for assessing diabetes risk.
Moreover, Lawrence et al (42) , in their study to estimate changes in prevalence of type 1 and type 2 diabetes in youths 19 years or younger in the US from 2001 to 2017, found that the prevalence of type 1 diabetes was an absolute increase of 0.67 per 1000 youths (95%, CI, 0.64-0.70) and a 45.1% (95% CI, 40.0%-50.4%) relative increase over 16 years; meanwhile, the prevalence for T2DM was an absolute increase of 0.32 per 1000 youths (95% CI, 0.30-0.35) and a 95.3% (95% CI, 77.0%-115.4%) relative increase over 16 years.
More alarming is that the prevalence of T2DM in youth is increasing with a high burden of target organ damage. Follow-up data from the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) (43) study show, at a mean age of 26 years (an average of 13 years after diagnosis), alarmingly high incidences of diabetes-related conditions: hypertension (68%), dyslipidaemia (52%), diabetic kidney disease (55%), and nerve disease (32%). Additionally, the incidence of retinal diseases increased from 14% to 51% in over just 7 years. While largely driven by obesity, unhealthy diets, and high levels of physical inactivity, the increasing prevalence of youth-onset (and adult) type 2 diabetes is also underpinned by socioeconomic, demographic, environmental, and genetic factors.
Regarding sedentary lifestyle, it is evident that sedentary behaviors constitute an attribute of the contemporary lifestyle and show a close relationship with various risk factors, in addition to cardiometabolic ones, such as bone health with a tendency to osteopenia, ACVD or cognitive deterioration, including increased risk of death (44-46). Indeed, high amounts of sitting time were associated with elevated likelihood of all-cause mortality and CVD in economically diverse settings, especially in low-income and lower-middle-income countries, according to a recently publication of the Prospective Urban Rural Epidemiology study, where a population-based cohort study included participants aged 35 to 70 years were recruited from January 1, 2003, and were followed up until August 31, 2021, in 21 high-income, middle-income, and low-income countries with a median follow-up of 11.1 years (47). Unlike physical activity programs, which involve time, transport, infrastructure, and logistics to consider, the reduction in sedentary behaviors can be achieved at a very low economic cost through simple micro-interventions, with no time limit, aimed at an increase in physical activity, modification of the sedentary habit and the implementation of activities with higher energy expenditure (48).
Health professionals, especially those dedicated to primary care or general practitioners, need to apply existing treatments in their proper dosage and as early as possible to obtain the maximum benefit and be vigilant in their adherence, as well as in strict observance of therapeutic changes in life habits. The key to success, most likely, lies in the early understanding of the pathophysiology of the cardiometabolic disorder, to be able to intervene biologically and behaviorally before a clinical outcome, which can eventually be fatal.
The clinical consequences derived from the increased cardiometabolic risk can be reflected in (1,15,30,31,49-52):
- Increased risk of CVD, as atherosclerosis is a ubiquitous condition. Generally, patients with vascular involvement in one arterial territory have atherosclerotic lesions in other arteries.
- High prevalence of T2DM and its entire clinical association with the highest risk of non-alcoholic fatty liver, cancer, and Alzheimer’s dementia.
- High frequency of arterial hypertension and arrhythmias such as atrial fibrillation.
- The impact and damage on target organs such as the heart, arteries, kidney, brain, and liver.
- Deterioration in quality of life, depending on the degree of disability with lower cardiorespiratory fitness.
- High mortality, especially sudden cardiac death which, in a high percentage of cases, is the first manifestation of cardiovascular disease.
Conclusion
Evidence has shown, without a doubt, that strict compliance with treatment (pharmacological and therapeutic changes in lifestyle, especially heart-healthy diet, and daily physical activity routine), reflected in excellent metabolic control (blood glucose, A1c, LDL-C and triglycerides) and blood pressure, can reduce the probability of a vascular event or progression to T2DM by more than 50%, ensuring a better quality of life (7,8). The care of cardiometabolic conditions requires the necessary facility to interact with patients in clear and understandable language, and instruct them about the benefits of existing approaches, as well as the risks of not complying with adherence to the prescribed treatment, or of following strategies and taking medications that are not duly proven, clearly warning that the objective is not only to control altered levels of blood glucose, lipids or weight, but also to prevent CVD, the final destination of these conditions when they are not treated on time and with the appropriate intensity.
Recommendations
High rates of overweight/obesity and prediabetes are found in young peoples studied and indicated the presence an increased cardiometabolic risk to develop ACVD and T2DM and associated complications. Thus, timely intervention is mandatory to identify age-appropriate strategies that address risks and to develop recommendations for routine screening of adolescents to identify those in risks. However, a more widespread public policy must be engaged in promoting healthy eating habits, more physical activity and avoid overweight and obesity no matter age or sex. The cardiometabolic continuum is an educational tool easy to apply in routine clinical practice.
Declaration
Acknowledgments
The authors would like to thank Gazi University, Department of Chemical Technology.
Conflict of Interest
The authors declare that they have no competing interests.
References
1. Mechanick JI, Farkouh ME, Newman JD, Garvey WT.(2020) Cardiometabolic-Based chronic disease, adiposity and dysglycemia drivers: JACC State-of-the-Art Review. J Am Coll Cardiol;75(5):525‐538
Publisher | Google Scholor
2. Arocha Rodulfo JI.(2021)Approach to the cardiometabolic continuum. Narrative description. Clin Investig Arterioscler. May-Jun;33(3):158-167.
Publisher | Google Scholor
