Atypical Presentation of Raynaud's Disease with Inferior Wall Infarct
Home / Journals / Atypical Presentation of Raynaud’s Disease with Inferior Wall Infarct / Articles In Press
Case Report
Atypical Presentation of Raynaud's Disease with Inferior Wall Infarct
Abstract
Introduction
Case Report
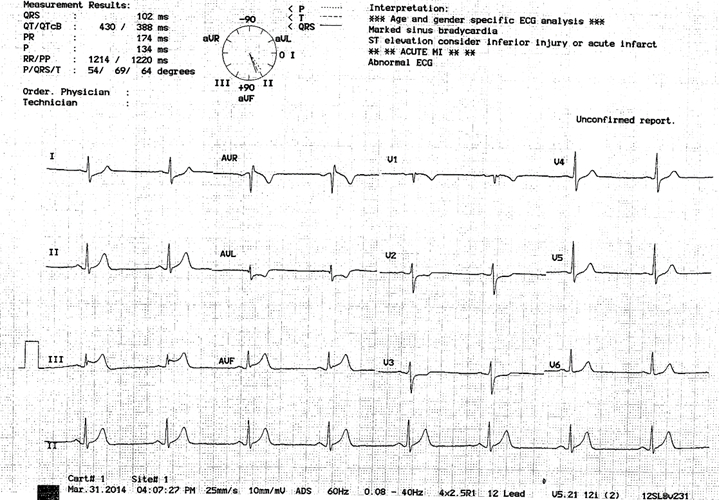
Figure 1: EKG of the patient showing ST segment elevation in leads II, III and AVF.

Figure 2: Image shows the discoloration of the patient’s fingers in response to cold.
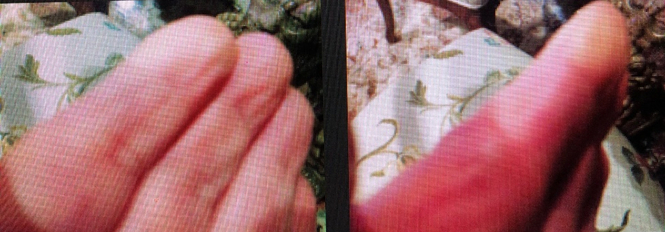
Figure 3: Image shows the blanching of patient’s fingers when exposed to colder temperatures.
Results
Materials and Reagents
Calcium fluoride (Sigma), used as an ionophore, Ag(I)S and CuS were commercially obtained. Anion and cation solutions (Merck) were obtained from solid salts. All solutions were prepared using twice purified water.
Instruments
An external Ag/AgCl reference electrode with a Jenway 3040 pH/ion meter was used for potential measurement. Potential values were measured at room temperature.
Preparation of fluoride selective electrode
A certain amount of the salt or salt mixture of Ag(I)S, CuS and CaF2 (10–15 mg) was taken and pellets were made by holding first under a pressure of 1940 atm for 1min, then pressure was increased to 7760 atm by adding each time 1940 atm for 1min. The pellets of 7mmdiameter were sealed with epoxy resin (0.7 g epoxy and 0.9 ghardener). To obtain a good sealing the epoxy resin on the edge of the tubing had to wait for about 10 min and then the pellet was sealed. One day after the pellet was sealed a silver wire is connected. For this purpose, the inside of the glass tube was filled to about 1 cm with a mixture of 0.5 g graphite powder and epoxy resin. The electrode prepared had to wait for about 2 days so that the resin can get dry. The surface of the electrode is washed and then polished with a soft paper [10].
Preparation of teeth samples
Four dental samples were taken from the faculty of dentistry. Tooth samples were kept in 5ml TISAB II (Total Ionic Strength Adjustments Buffer) for 24 hours. The amount of fluoride passing into the solution was measured using an electrode.
Discussion
The prevalence of Raynaud’s phenomena varies widely between populations. In the US, it is estimated that up to 200,000 people are affected. A higher prevalence among other populations, such as France, is found (3). Raynaud’s phenomenon can be either a primary phenomenon or secondary to various underlying medical disorders and drug-related conditions.
Vasospastic angina, previously called Prinzmetal or variant angina, is a form of abnormal vascular response to various stimuli. Prinzmetal et al (4) initially described a clinical syndrome that manifested as rest angina associated with ST-segment elevation that promptly responded to sublingual nitrates. Since this differs from classical angina described by Heberden (effort angina associated with ST depression) (5), he referred to it as variant angina.
The correlation between vasospastic angina and Raynaud’s has been explained previously in literature (6,7). Miller et al (6) reported a high prevalence of Raynaud’s phenomenon in patients with vasospastic angina occurring at a rate of 24% in patients with variant angina as compared to 3% and 5% in controls (p-value<0.01). Hence vasospastic angina in some patients is a manifestation of a generalized vasospastic disorder and could be associated with migraine, Raynaud’s phenomenon, and aspirin-induced asthma (8).
Coronary vasospasm can occur in patients with normal coronary arteries as well as in patients with atherosclerosis. However, it is still poorly understood whether coronary vasospasm can promote atherosclerotic alterations or whether the latter may predispose to spasm (9).
The patient described in our case has a typical history of Raynaud’s phenomenon diagnosed clinically, along with recurrent attacks of chest pain relieved by nitrates that were thought to be due to vasospastic angina. However, coronary angiography revealed atherosclerotic narrowing with 80% occlusion of the right coronary artery. This finding was similar to an autopsy result in one of the patients described in Prinzmetal et al paper (4), which revealed that the right coronary artery (which presumably had caused resting angina with ST elevation in inferior leads) had an 80% stenosis. This observation led to the conclusion that coronary spasm was associated with atherosclerosis. Later it was found that coronary spasms can also occur in patients with angiographically normal coronary arteries (10).
Recent experimental studies demonstrate that several endothelium-derived factors mediate vascular smooth muscle cell tone and that damaged endothelium may play a major role in the pathogenesis of vasospasm (11). Endothelial damage may occur even in the early stages of atherosclerosis. Zeiher et al (12) indicated that abnormal vasoconstriction was observed in early atherosclerotic sites in patients without variant angina using intra-coronary ultrasound. Yamagishi et al (13) reported that early stages of atherosclerosis were observed by intracoronary ultrasound at the site of spasm in patients with variant angina, even in the absence of an angiographically significant coronary disease. However, these results were challenged by a porcine model of spasm, indicating that endothelial vasodilator function was preserved at the spastic site (14); it remains to be elucidated.
It was suggested that endothelial dysfunction with decreased nitric oxide release and reduced bioavailability combined with vascular smooth muscle cell hyperreactivity might be important in developing coronary spasm. However, endothelial dysfunction alone might not be sufficient to explain vasospastic angina (15). Therefore, more studies need to be done to understand the pathophysiology associated with the vasospasm associated with Raynaud’s disease.
Conclusion
References
- Hegazy MA, Kamal S Mansour KS, Alzyat AS, Mohammad MA, Hegazy AA. (2022). Myocardial Infarction: Risk Factors, Pathophysiology, Classification, Assessment and Management. Cardiology Research and Reports. 4(5).
- Bosson N, Isakson B, Morgan JA, Kaji AH, Uner A et al (2019)Safety and Effectiveness of Field Nitroglycerin in Patients with Suspected ST Elevation Myocardial Infarction. Prehosp Emerg Care. Sep-Oct;23(5):603-611.
- Maricq HR, Carpentier PH, Weinrich MC, Keil JE, Palesch Y et al (1997) Geographic variation in the prevalence of Raynaud’s phenomenon: a 5 region comparison. J Rheumatol. May;24(5):879-89. PMID: 9150076.
- Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N.(1959)Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med. Sep;27:375-388.
- Silverman ME. William Heberden and Some Account of a Disorder of the Breast. Clin Cardiol. 1987 Mar;10(3):211-213
- Miller D, Waters DD, Warnica W, Szlachcic J, Kreeft J (1981) Is variant angina the coronary manifestation of a generalized vasospastic disorder? N Engl J Med. Mar 26;304(13):763-766.
- Robertson D, Oates JA.(1978) Variant angina and Raynaud’s phenomenon. Lancet. Feb 25;1(8061):452.
- Contreras Zuniga E, Gomez Mesa JE, Zuluaga Martinez SX, Ocampo V, Andres Urrea C.(2009)Prinzmetal’s angina. Arq Bras Cardiol. Aug;93(2):e30-2.
- Ong P, Aziz A, Hansen HS, Prescott E, Athanasiadis A (2015) Structural and Functional Coronary Artery Abnormalities in Patients With Vasospastic Angina Pectoris. Circ J.;79(7):1431-1438. Epub 2015 Jun 18.
- Cheng TO, Bashour T, Kelser GA Jr, Weiss L, Bacos J.(1973) Variant angina of Prinzmetal with normal coronary arteriograms. A variant of the variant. Circulation. Mar;47(3):476-485.
- Ganz P, Alexander RW. (1985) New insights into the cellular mechanisms of vasospasm. Am J Cardiol. Sep 18;56(9):11E-15E.
- Zeiher AM, Schächlinger V, Hohnloser SH, Saurbier B, Just H. (1994) Coronary atherosclerotic wall thickening and vascular reactivity in humans. Elevated high-density lipoprotein levels ameliorate abnormal vasoconstriction in early atherosclerosis. Circulation. Jun;89(6):2525-2532.
- Yamagishi M, Miyatake K, Tamai J, Nakatani S, Koyama J et al (1994) Intravascular ultrasound detection of atherosclerosis at the site of focal vasospasm in angiographically normal or minimally narrowed coronary segments. J Am Coll Cardiol. Feb;23(2):352-357.
- Miyata K, Shimokawa H, Yamawaki T, Kunihiro I, Zhou X et al (1999) Endothelial vasodilator function is preserved at the spastic/inflammatory coronary lesions in pigs. Circulation. Sep 28;100(13):1432-1437.
- Picard F, Sayah N, Spagnoli V, Adjedj J, Varenne O. (2019) Vasospastic angina: A literature review of current evidence. Arch Cardiovasc Dis. Jan;112(1):44-55.
Disclosures
No relevant conflicts of interest to declare.
